What is Posterior Uveitis?
Uveitis is an inflammation of the inside of the eye, specifically the layer of the eye called the uvea. (See What is Uveitis? fact sheet). Nowadays the term is used to describe inflammation that affects both the uvea and other structures inside the eye such as the retina. The terms 'Intra-Ocular Inflammation' or 'Ocular Inflammatory Disease' are often come across as alternative names to uveitis.Uveitis is an 'umbrella' term for several quite different conditions. These conditions are so diverse that they can be classified, or put into groups, in a number of different ways:
Examples are:
- Infectious or non-infectious
- Acute or chronic
- Endogenous or exogenous (meaning coming from inside or outside the body).
- Located at the front (anterior), middle (intermediate), or back (posterior).
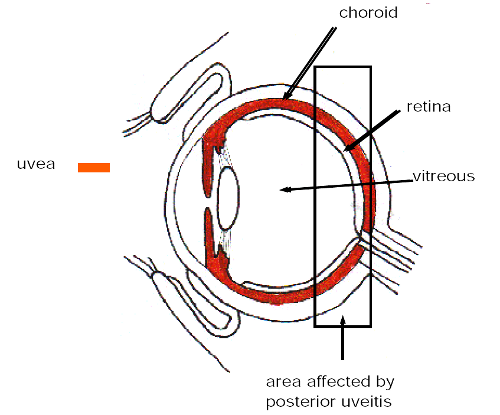
Posterior uveitis, affects the back of the eye. That part of the uvea is
called the choroid. (see diagram next page). An inflammation in the
choroid would be called choroiditis. The inflammation may also arise in,
or affect, the retina (retinitis) or in the blood vessels at the back of
the eye (vasculitis).
 Posterior uveitis describes where the uveitis is. It is not really a
disease in itself. In fact there are a large number of uveitic
conditions which can be described as posterior uveitis. For anyone
reading up about their condition, posterior uveitis is a useful term
because it has features which are different from anterior uveitis, the
most common form of uveitis.
Posterior uveitis describes where the uveitis is. It is not really a
disease in itself. In fact there are a large number of uveitic
conditions which can be described as posterior uveitis. For anyone
reading up about their condition, posterior uveitis is a useful term
because it has features which are different from anterior uveitis, the
most common form of uveitis.
The most typical features of Posterior uveitis are:
- It is usually painless
- It is more likely to impair the vision
- Floaters are common
- Vision can be impaired suddenly or reduce gradually over a period of time.
Causes of Posterior Uveitis
As already stated there are a variety of conditions which can be described as posterior uveitis. They all may have quite different causes. It is not really helpful to try to define the cause of posterior uveitis as such. It is best to deal with each separate condition (see examples further on in this sheet). Posterior uveitis may be caused by the full spectrum of different possibilities, like infection with viruses, fungi, parasites, autoimmune disease or trauma.Treatment of Posterior Uveitis
Although this, again, will vary according to the type of posterior uveitis, there are certain general differences between the treatment of posterior, intermediate or anterior uveitis. The main difference arises from the ease in which the drugs used to treat the condition can be delivered to the area of inflammation.- In anterior uveitis, the inflammation is near the front of the eye and eye drops can reach the source of the inflammation.
- In intermediate uveitis, eye drops may well be able to reach the area of inflammation and sometimes injections around the eye can also be used to "deliver" the drugs where they are needed, slightly further back in the eye.
- In Posterior uveitis, the inflammation is at the back of the eye and drops simply won't reach the affected area. This requires a different approach and this is why the same drugs, (usually a steroid) are taken systemically (in tablet form). If the posterior uveitis is caused by a virus then the same applies; the antiviral drug will be taken by tablet or injection, instead of by drops.
Although this is an over simplification of the treatment of uveitis, it should explain why some forms of treatment are chosen for one case and not considered for others.
This systemic type of treatment will result in the drugs affecting the "whole body", unlike the eye drops or injections. This means that there will be more likelihood of unwanted side effects. It is very important from the patient's point of view to be aware of this. The choice to use systemic drugs when offered by the doctors is likely to be the correct one. However it is of enormous benefit to all involved if the patient is aware of the balancing act that exists between benefit and risk.
At the end of the day, if as patients, we can find out a little about the benefit and risk "equation" and accept for ourselves that the benefits outweigh the side effects, then we are going to get on much better with our treatment and have few doubts about it. It also allows us to accept the side effects a little easier.
If, of course, the balance seems to be going the other way then we must discuss this with our doctors. (see also the fact sheet: The treatment of uveitis in 'essential background').
As stated earlier, Posterior uveitis is a term covering several conditions. It may be useful if you have been given a name for a condition to know whether it may be described as a Posterior uveitis. Below then is a list of some types of posterior uveitis or medical conditions associated with it.
- Behçet's Disease
- Sarcoidosis
- Idiopathic retinal vasculitis
- Vogt-Koyanagi-Harada Syndrome
- Acute posterior multifocal placoid pigment epitheliopathy (APMPPE).
- Presumed ocular histoplasmosis syndrome (POHS).
- Birdshot choroidopathy
- Multiple sclerosis
- Sympathetic Ophthalmia
- Punctate inner choroidopathy
- Toxoplasmosis
Whilst it is important to be able to 'pin down' the exact diagnosis of uveitis it does not always work out like that because of the great variety of ways this condition presents itself. Our eye specialists aim to identify and treat sight threatening inflammation. This may take different forms. For example:
- Macular oedema (accumulation of fluid in the central part of the retina)
- Vasculitis (inflammation of the blood vessels of the retina).
- Vitritis (inflammatory cells in the vitreous gel: we see as floaters).
- Sub-retinal neovascularisation (formation of new blood vessels).

